
How Historical Inequities Shape the Course of Pandemics
By
Nadja Durbach
PROFESSOR OF HISTORY
Gregory Smoak
ASSOCIATE PROFESSOR OF HISTORY
AND DIRECTOR OF THE AMERICAN WEST CENTER
We can never view pandemics as purely biological events. While it is true that microbes are discrete organisms, replicating and mutating through natural processes beyond our control, human actions and power structures have always shaped the epidemics those pathogens have spawned. This is as true today as it was when relentless waves of disease first began to devastate Native peoples in the centuries following European contact. Native peoples were subject to dozens of distinct epidemics that included bubonic plague, measles, typhus, influenza, and smallpox. Pre-contact
Above Left: Sixteenth-century Aztec
drawings of smallpox and measles
victims
Below: Nurses working in the Red
Cross rooms in Seattle, WA, with
influenza masks on faces, 1918
▼
was marked by warfare, social dislocation, slave raiding, and the destruction of Native
subsistence bases. Malnutrition was in fact the single greatest factor in spiking
epidemic mortality rates. The kind of health care infrastructure that we may take
for granted today did not exist; caring for the afflicted was the responsibility of
kin and community. Regardless of biological immunity, any society in collapse, unable
to feed or heal itself, stands little chance in the face of a pandemic. Still, generations
of Euro-Americans cited high Native mortality rates as evidence of inherent Native
weakness, displacing blame.
Native peoples were not the only Americans subject to racist discourses and actions
that shaped their experience of epidemic disease. When yellow fever hit Philadelphia
in 1793, esteemed doctor Benjamin Rush, one of the signatories of the Declaration
of Independence, theorized that African Americans were immune to the disease. While much
of Philadelphia’s white population attempted to self-quarantine, its free Black people
were
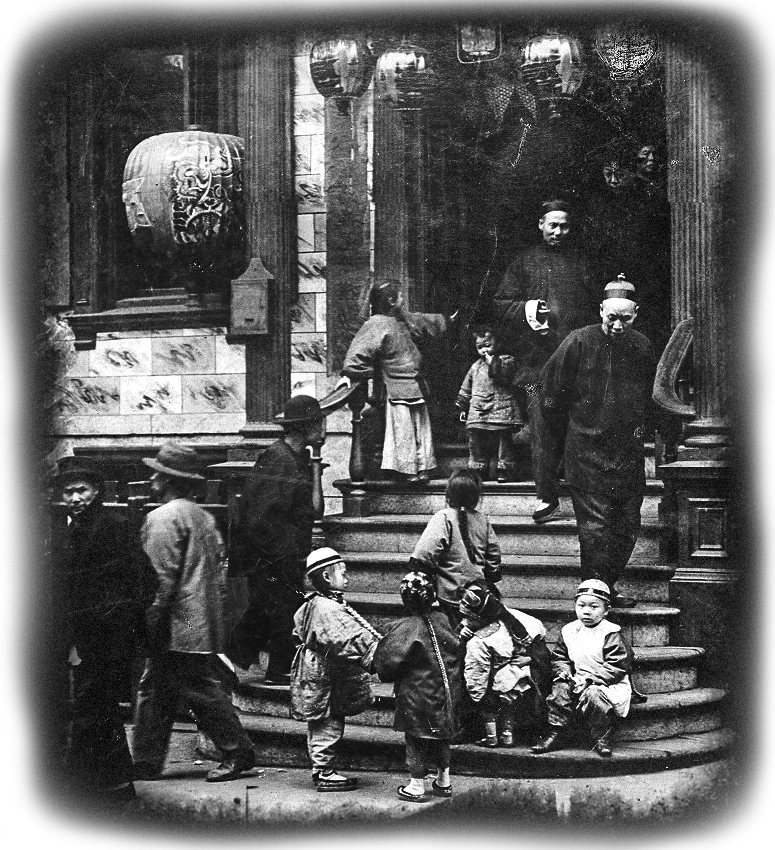
Above: San Francisco's Chinatown c. 1900. Photo by Arnold Genthe
Below: Black people struck by the Spanish Flu of 1918 received substandard care in segregated
hospitals.
▼
recruited to be first responders: they were put to work as nurses, coffin makers,
and grave diggers, coming into direct contact with contagious bodies. While at least
240 African Americans died of the disease, debunking Rush’s theory, they were nevertheless
accused of profiteering and looting rather than being praised for doing the dangerous
work of caring for the sick and the dead.
Since the early 19th century, immigrants to the United States whose “whiteness” was
always contested, have also been blamed for pandemic diseases. In the 1830s and 40s,
when they arrived in America seeking economic opportunity and fleeing devastating
famine, the Irish—considered both racially inferior and as Catholics widely despised
by the majority Protestant population —were accused of spreading cholera. The Jewish
refugees from Eastern Europe who passed through Ellis Island around the turn of the
century
in the wake of anti-Semitic programs
During the last great global pandemic —the influenza of 1918-1919—worldwide, some half a billion people were infected and up to 50 million died. In the United States,
Native peoples were hit harder than any other population. Nearly one quarter of all
people living on reservations came down with influenza between October 1918 and March
1919, and 9 percent died. That was quadruple the death rate in America’s largest cities.
The influenza of 1918 was particularly devastating for the Navajo people. An estimated
40 percent fell ill and at least 2,000 Navajos out of a population of just over 30,000
died. Rather than blaming preexisting conditions, malnutrition, and lack of adequate
health care for the mortality rate, many physicians, scientists, and government officials
interpreted the death toll as evidence of the genetic inferiority and bodily weakness
of a “primitive race.”
It is no surprise to historians that this
novel virus is now ravaging the United States’ least privileged and most vulnerable communities. In 2020, the Navajo Nation is again at the center of this pandemic. Some 175,000 people currently live on the Navajo Nation, an area the size of West Virginia, whose infection rate is nevertheless almost double that of New York state. Many of the same circumstances that spiked Navajo morbidity and mortality a century ago are still factors today. Preexisting conditions such as diabetes and heart disease and limited access to health care have made COVID-19 a deadly threat to this community in particular and reveal how historical inequities continue to shape the course of pandemics. Like the African Americans that Rush conscripted as first
At the same time as we invest in containing the spread of this virus... we should thus attend to the lessons of the past.
The Navajo Monument Valley Tribal Park in Oljato-Monument Valley, UT, closed to the
public in an effort to prevent the spread of COVID-19 on the Navajo reservation (source)
▼
